Switch to the mobile version of this page.
Vermont's Independent Voice
- News
- Arts+Culture
- Home+Design
- Food
- Cannabis
- Music
- On Screen
- Events
- Jobs
- Obituaries
- Classifieds
- Personals
Browse News
Departments
Browse Arts + Culture
View All
local resources
Browse Food + Drink
View All
Browse Cannabis
View All
-
Culture

'Cannasations' Podcaster Kris Brown Aims to 'Humanize'…
-
True 802

A Burlington Cannabis Shop Plans to Host…
-
Business

Judge Tosses Burlington Cannabiz Owner's Lawsuit
-
Health + Fitness

Vermont's Cannabis Nurse Hotline Answers Health Questions…
-
Business

Waterbury Couple Buy Rare Vermont Cannabis License
Browse Music
View All
Browse On Screen
Browse Events
Browse Classifieds
Browse Personals
-

If you're looking for "I Spys," dating or LTRs, this is your scene.
View Profiles
Special Reports
Pubs+More
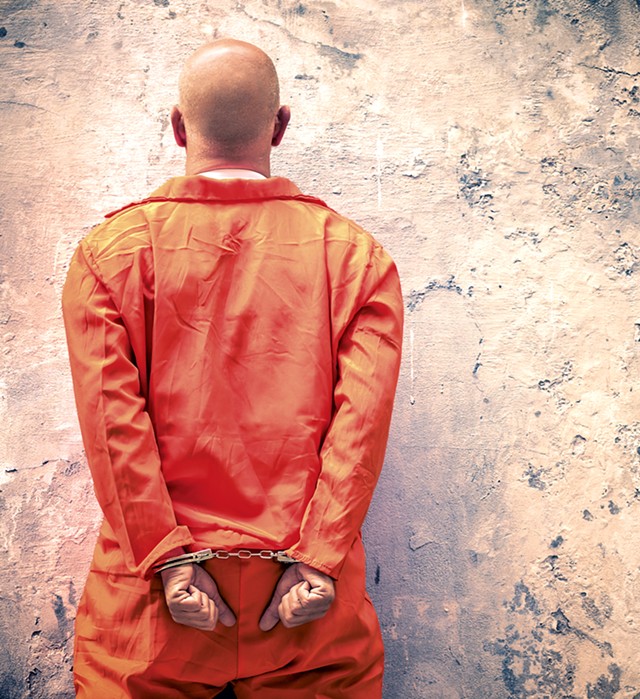
How Drug Treatment Policies in Vermont Prisons Contribute to the Opiate Crisis
Published November 1, 2017 at 10:00 a.m. | Updated December 12, 2019 at 3:15 p.m.
Sam Blatt tried OxyContin as a freshman at Castleton State College. Three years later, he was in prison for burglary and writing bad checks — crimes fueled by a heroin addiction that had quickly consumed him.
When he got out in 2014, Blatt moved to Winooski with his girlfriend and found a construction job. Thanks to a daily dose of methadone, he was clean.
Then, about three months after his release, Blatt did cocaine at a Fourth of July party. After confessing to his parole officer, he was sent back to prison, where medical staff promptly took him off methadone for "pissing dirty," as he put it.
"I hadn't used any heroin at the time. None. Zero," Blatt recalled, incredulously. "I did cocaine one time and told them about it."
He spent the next month detoxing from methadone in a small cell with a thin mattress and a metal toilet. "I didn't sleep for like 25, 30 days straight. I'd just roll around. My legs would ache so bad. My anxiety was through the roof.
"It's literally torture," he continued. "I'd rather die."
Vermont is in the midst of an opiate addiction crisis, yet its correctional facilities routinely deny inmates treatment — a practice many say drives addicts back to street drugs and crime.
"It is literally killing people," said Tom Dalton, executive director of Vermonters for Criminal Justice Reform. "I'm aware of multiple incidents where people have been taken off their medication while incarcerated, or where the transition from incarceration to treatment in the community left a gap that resulted in somebody overdosing and dying."
The Vermont Department of Corrections does offer limited "medication-assisted treatment" (MAT). All seven of the state's prisons administer opioid medications that diminish cravings and temper the side effects of heroin withdrawal: specifically, methadone and buprenorphine, aka Suboxone. To maintain normal lives, patients often stay on those medications for long periods of time. Multiple studies have shown that, combined with substance abuse counseling, they are the most effective remedy for opiate addiction.
But no Vermont jail offers treatment for more than 90 days, and it's only available to inmates with existing prescriptions; other incarcerated addicts go into immediate withdrawal. Also, anyone who qualifies for MAT can lose the "privilege," as a nursing administrator at one Vermont prison referred to it, for breaking the rules.
The treatment is supposed to conclude with a "compassionate medical taper," according to DOC Commissioner Lisa Menard, which gradually reduces the dose of buprenorphine or methadone over a period of days or weeks. But Seven Days spoke with seven current and former inmates who said people are sometimes cut off "cold turkey."
"Kevin" was taking 90 milligrams of methadone in March when he got a 15-day jail sentence for using cocaine. The Colchester resident, now 41, asked for anonymity because he's having trouble finding a job and doesn't want to hurt his prospects.
"I said to the nurse, 'OK, so what kind of a taper are you going to give me?'"
Her response, as he recalled it: "Oh, we're not going to taper you."
"I just about came unglued," said Kevin.
A few days into his detox, he began getting what he calls the "creepy-crawlies" — a sensation that "feels like your skin is crawling off you." He couldn't keep down food and had diarrhea so severe that "if you take a step, and you put your foot down too hard, you gotta change your pants."
Sharing his one-room cell with another inmate didn't make it any easier.
"I had one shower in 15 days," Kevin continued, explaining that he couldn't summon the energy to leave his cell. The pain wasn't merely physical; he experienced intense anxiety. "It makes you go cuckoo," he said.
Officials across the political spectrum now refer to the opiate epidemic as a public health crisis, not a criminal scourge. President Donald Trump has joined the chorus and last week directed the U.S. Department of Health and Human Services to declare a short-term public health "emergency."
But the Vermont DOC apparently didn't get the memo.
Rep. Selene Colburn (P-Burlington) said she believes "People should be allowed to continue their methadone and Suboxone medication in prison just as they would any other medication."
Echoing her sentiment, Kevin noted, "They don't take the insulin away from the diabetics."
Drug Resistant
Methadone has been around since 1972, but Vermont — in particular, its prisons — has taken decades to embrace the narcotic medication.
Vermont was one of the last states to establish a methadone treatment clinic. The state's former governor, Howard Dean, a physician, initially opposed lawmakers' attempts to create one, citing a concern that endures today: that methadone would become a "street drug," ensnaring patients in another form of addiction.
Dean eventually reached a compromise with the legislature, and the state's first community clinic opened its doors in October 2002 in Burlington.
In an interview last week, Dean said he never opposed medication-assisted treatment, but, at the time, he favored buprenorphine over methadone, believing it was harder to abuse. Buprenorphine, which was in clinical trials at the University of Vermont School of Medicine, didn't get U.S. Food & Drug Administration approval until 2002.
Lawsuits and legislation are largely responsible for the current prison treatment program. Pregnant inmates have been receiving methadone for at least two decades, according to Menard, but other inmates have had a harder time gaining access to the medication.
In 1999, Putney resident Keith Griggs, who was battling heroin addiction, was arrested for forgery. He avoided jail time with a plea agreement that required him to continue receiving methadone treatment. Since Vermont didn't have a clinic at the time, he drove or hitchhiked to Greenfield, Mass., every day to get his 200-milligram methadone dose.
When a parole violation landed Griggs in jail for a two-week sentence in 2001, the Vermont DOC refused to give him his methadone. Griggs sued, and in an emergency hearing, a Windsor Superior Court judge ruled that he was entitled to get his meds. The DOC lost on an appeal to the Vermont Supreme Court and then opted to release Griggs early rather than provide his medication.
Two months later, an inmate named Shawn Gibson sued and lost, but his circumstances were slightly different: His methadone treatment wasn't court-ordered, and his prison stay was longer than two weeks.
Citing these lawsuits in a 2003 article in Vermont Law Review, Rebecca Bouchard made the case that "denying methadone to inmates can no longer pass constitutional muster ... It is deliberate indifference to serious medical needs, it offends evolving standards of decency, and it is cruel and unusual punishment."
In 2004, the DOC did establish guidelines allowing inmates to receive treatment for up to 30 days, but those guidelines made clear that the department was not conceding that "access to methadone is required by prevailing medical standards or that abrupt methadone detoxification in a correctional setting is not within prevailing medical standards."
Dr. John Brooklyn, who cofounded Vermont's first methadone clinic, said health officials began meeting with DOC officials in 2006 or 2007 to discuss offering more in-prison treatment. But little came of the talks, and treatment guidelines remained unchanged in the next few years, according to DOC officials.
Then in early 2013, a man who had just finished a two-week jail sentence overdosed on heroin and died. He had been six years sober, but the DOC took him off his methadone in prison, according to Dalton, director of Howard Center's Safe Recovery program at the time. Privacy policies prevented him from revealing the man's name.
"That was the final straw," said Dalton. He began lobbying lawmakers to expand treatment in prison. Criminal justice reform advocate Suzi Wizowaty, a state representative at the time, championed the cause, and, by the end of the 2013 session, the legislature had created a work group to study the matter.
In a report submitted in November 2013, that group, which included Dalton and officials from the departments of health and corrections, proposed a one-year pilot program that would provide inmates with methadone or buprenorphine for up to a full year. This was the first time that "bupe," as it's called, would be offered in Vermont prisons.
The DOC didn't start the pilot until October 2014, and, when it did, the scope was more modest. The department had decided to offer treatment for up to 90 days at just two of its seven facilities: Chittenden Regional Correctional Facility in South Burlington and Northwest State Correctional Facility in Swanton.
According to DOC data, 98 percent of the 413 pilot-project participants stayed on treatment until their release or for the full 90 days; only 2 percent were taken off for noncompliance.
The work group deemed the pilot a success in its follow-up report, submitted to the legislature in November 2016, and recommended providing up to 120 days of treatment at all of the state's prisons.
One year later, nothing has changed: The 90-day policy remains in place at the facilities in South Burlington and Swanton; the other five prisons still adhere to a 30-day maximum.
'It's a Privilege'
Ten inmates sit quietly in chairs arranged in a circle, cloaked in black barber gowns, their hands pinned under their buttocks. A guard stands sentry as a nurse makes the rounds. She gives each prisoner a dose — crushed tabs of buprenorphine or a small bottle of methadone — like a priest administering communion. After 15 minutes, the inmates are instructed to drink a cup of water. The nurse comes around again to check their mouths to make sure they've swallowed their meds.
That's how inmates, officials and corrections protocol describe the daily distribution of medicine-assisted treatment in Vermont jails, a ritual off-limits to a reporter. The cloaks, the waiting, the water, the hands and the mouth checks are all intended to prevent prisoners from "diverting" meds. Prisoners still find ways to circumvent these measures, said Jennifer Sprafke, assistant superintendent of security at Chittenden Regional, which is Vermont's only women's prison.
One tactic is to vomit up the medication, and then sell it, Sprafke noted.
Bupe, which can provide a muted high, is the most common form of contraband in Vermont prisons, according to Menard.
That's why bringing more of these meds into prison sounded like a bad idea to corrections officers in 2013, when the state started talking about expanding treatment. But during an interview in her Waterbury office, Menard said this diverted medication hasn't turned out to be a problem; unauthorized bupe is primarily smuggled in from the outside.
Many see bupe's prevalence in prison as a sign that inmates are self-medicating, and even Menard is willing to entertain the theory that the black market for it would dry up if everyone seeking treatment could get it.
Those lucky enough to have an active prescription still need DOC approval to continue taking it. Medical professionals make those decisions on a case-by-case basis, said Ben Watts, the DOC's health services administrator.
If the inmate is taking methadone, the DOC's health services staff will consult with the physician who prescribed it, but they don't have to follow the community doctor's recommendation. In the case of buprenorphine, the DOC becomes the prescriber and sole decision maker.
The top three reasons it terminates treatment are: The inmate's "expected length of stay" exceeds 30 days — or 90 days, in the case of South Burlington or Swanton; he or she was seen, or is suspected of, diverting drugs; or a urine test turned up another illicit drug that is not marijuana.
But former inmates said it's not that simple. They report that some DOC staff use medication-assisted treatment to control behavior. When they took him off methadone, Kevin said it was "almost like a punishment."
"It's not a medication to them; it's a privilege," William McGuinness, a 37-year-old South Burlington resident who's done multiple prison stints, said during an interview in August at a Burlington coffee shop.
As if on cue, Crystal Alexander, the nursing supervisor at Chittenden Regional, said those very same words — "It's a privilege" — on a tour of the facility last week.
Once revoked, it's not easy to get treatment back. Alexander noted that a woman had recently come into prison with a prescription for bupe, and, even though her urine test came back clean, she was taken off her medication because she'd diverted her bupe during a previous prison stay.
Menard said people get disqualified for drug-positive urine tests because illicit substances mixed with methadone or bupe constitute "a health and safety risk."
This explanation doesn't make sense to some health professionals outside the prison walls. "You walk in the door at DOC, and it's become practice now for them to not continue to treat you for reasons that I am still trying to understand," said Brooklyn, who is medical director at South Burlington's Chittenden Clinic, which provides both methadone and buprenorphine to patients.
His clinic continues to treat people when they have illegal drugs in their system because "the alternative is worse," Brooklyn said. Terminating treatment may lead them back to heroin or other street drugs, which could result in an overdose.
Just because someone is still using — even if it's heroin — doesn't mean they're not committed to their recovery, Brooklyn noted. "Maybe they've gone from injecting 50 times a week to two times a week," he said. "We look at that as a significant improvement."
28 Days in Hell
Vermont inmates are weaned from medication-assisted treatment with a "compassionate medical taper," according to Menard, but they still go through withdrawal. Symptoms set in within eight to 30 hours of the last dose and can include sweating, involuntary twitching and anxiety. After a few days, people often experience diarrhea, nausea, vomiting, stomach pain, aches and cramps, and insomnia.
The experience is exponentially worse when an addict's drug supply ends abruptly. A number of current and former inmates said that's what happened to them in Vermont jails.
Soft-spoken McGuinness, who sheepishly admitted to being a car thief, said he went 28 days without sleeping for more than an hour at a time. His drug problems started when he was 17, deejaying parties and doing ecstasy.
"They basically throw you in a cell, and you're shaking, you're shitting yourself," McGuinness summarized. "I get severe back pain. I can't even move. I'm super weak. I get hot and cold chills."
"I've attempted suicide in there over that," said Jimmy Vezina, a 42-year-old lifelong resident of Burlington who said he was injecting cocaine by the time he was 13.
Several former inmates said they've witnessed other mid-detox suicide attempts. Kevin said a man in the cell opposite his tried to hang himself with a bedsheet. "He told them in the nurses' office, 'Listen, if you don't put me back to my normal dose, I'm stringing up,' and that night, the lights come flying on, and he'd strung up in a corner of his room." Guards cut him down before it was too late.
Watts said that the DOC follows the Clinical Opiate Withdrawal Scale for all inmates going through detox. Guards check on inmates every 15 minutes, and health service staffers check their vitals every six hours. They offer various medications to ease the symptoms: clonidine for anxiety and muscle aches; hydroxyzine for nausea and vomiting; Imodium for diarrhea; and Tylenol for general pain.
Kevin's take: "Their protocol is Imodium, aspirin or Tylenol, and 'Here's an extra blanket; have a good day.'"
"The medical support for the detox is minimal at best," said Dalton. "There's a lot of avoidable suffering that is happening."
Statewide, an average of 73 Vermont inmates receive medication-assisted treatment per month, and 55 are going through withdrawal.
Menard said she couldn't comment on specific cases but acknowledged that she does get calls from inmates' family members who are concerned about their detox experiences.
Watts, who reviews written complaints when they come in, said, "I can tell you that nine times out of 10 ... we determine that the complaint is not founded in the sense that any policy or procedure was violated. It's just more that the patient was upset that their medication wasn't continued."
Detoxing from methadone or buprenorphine rarely results in death, but it's almost always excruciating and can last for as long as a month. Heroin withdrawal wraps up in 10 days.
That's why, after six months behind bars, Blatt returned to heroin instead of methadone. "I was, like, I'm not getting back on, because if I do slip up ... they're just going to take me off it, anyways." Several months later, he was back in prison for burglarizing student dorms at UVM.
In September, in the living room of his Burlington sober house, the 26-year-old told a reporter that he'd gotten clean again, this time with bupe. "I'll never take methadone again after that," he said.
When Vezina got out last year, he, too, reverted back to heroin. "I ended up using only two bags and I OD'd and almost died ... They really did hit me with the adrenaline and everything. Three shots of Narcan [an overdose-reversing drug]. Doctors said another minute or less without air, and I would have been brain-dead."
Vezina is now back on buprenorphine, but, in the back of his mind, he still worries about going through another detox. "It makes me afraid to take my bupe every day, because what if I do relapse?" Sitting on a bench in Burlington's City Hall Park, he paused in the middle of a sentence to point out a man smoking crack.
Vermont Department of Health data shows that, from January 2014 through March 2017, at least 12 percent of all reported overdoses involved someone recently released from jail. A 10-year study in Washington State found that former inmates are 130 times more likely than the general population to overdose in the two weeks after they're released from prison.
"Their highest risk for overdose and death is the day they walk out of prison," said Dr. Brooklyn. With the recent proliferation of fentanyl, a highly potent opiate, that risk is even higher.
Those statistics worry Erika Hagen. The talkative 26-year-old takes methadone every day — she's been clean for four months — and works full time. But her boyfriend, Andrew Lavallee, is battling his heroin addiction behind bars. Lavallee, 32, was jailed May 20 after evading police during a high-profile car chase that ended at the Burlington waterfront. Hagen was in the passenger's seat.
According to Hagen, Lavallee had been getting his methadone until July, when the DOC abruptly terminated it because staff said they saw her spit buprenorphine into his hand during a prison visit — something she says didn't happen.
"My fear is, he's gonna crave to get high, and he's gonna come out of there and use, and he's gonna overdose and die," Hagen said. "DOC is setting them up to fail."
'Ahead of the Curve'
Alexandra Fusco has a different complaint about her most recent Vermont jail stay: the lack of substance abuse counseling. Although federally mandated at community clinics, it is not a requirement in correctional facilities where medication-assisted treatment is only provided on a temporary basis.
The 28-year-old says she was introduced, and became addicted, to heroin in 2014 while spending 22 months in prison. She was there for having sexual contact with a boy under the age of 16 while she was a residential counselor at the Bennington School.
After an unsuccessful stint in rehab, her furlough was revoked, and she's been back in prison since July. Calling from jail on October 23, Fusco said she's doing her best to stay clean despite getting little support from the facility. For more than three months, the only drug counseling she could access was a Sunday evening Alcoholics Anonymous meeting, and sometimes even that, capped at 20 people, wasn't an option.
In mid-October, Fusco finally got off the waitlist for an in-prison drug counseling program, run by an outside organization called Phoenix House and unique to the Chittenden prison. She now attends group meetings, receives individual counseling for 30 minutes every two weeks and participates in mindfulness classes twice a week. Fusco described the program as understaffed and unstructured.
"I don't think we're doing as much as we could be," conceded state Sen. Dick Sears (D-Bennington), who supports making medication-assisted treatment and counseling available to all inmates without time limits. But "we're ahead of the curve compared to other states," the judiciary committee chair pointed out.
Nearly every official Seven Days spoke with made the same observation when asked about the state's treatment offerings. And they're right — a 2016 Pew Charitable Trusts survey reported that fewer than 40 U.S. prisons provide methadone or buprenorphine.
Still, one doesn't have to travel far to find more comprehensive programs. Since 2016, Rhode Island has provided treatment to any inmate who qualifies, and Connecticut is in the process of implementing long-term treatment programs at all of its prisons.
Correctional facilities in Canada, Europe, Australia and the United Kingdom have been providing medication-assisted treatment for years.
Earlier this year, Trump's commission on combatting drug addiction and the opioid crisis recommended expanding treatment in correctional facilities, noting in its report that "multiple studies have shown that individuals receiving MAT during and after incarceration have lower mortality risk, remain in treatment longer, have fewer positive drug screens and have lower rates of recidivism."
Two years after the start of the pilot, and one year after the work group recommended expanding treatment to up to 120 days in all seven Vermont correctional facilities, state officials are saying they're now ready to expand treatment — but only to 90 days.
The DOC pays for the medication-assisted treatment program out of its own budget because Medicaid won't pay for inmates. It spends about $600,000 per year on the program, according to Watts, and expanding it to 90 days in all prisons would increase the price tag by $180,000. Menard, who supports the move, says they can cover the cost within their current budget.
"In a situation where almost no state offers any treatment, 90 days is revolutionary," said Vermont Health Commissioner Dr. Mark Levine.
But not everyone is so impressed.
"I think we have to be careful to both acknowledge progress, but also not to be too quick to congratulate ourselves when people are dying," Dalton said. "We don't want half measures at this point and that's a half measure."
Howard Center chief executive officer Bob Bick delivered a gentler rebuke. "I think there's an opportunity for the Department of Corrections to move forward and take a more assertive approach at creating access to treatment within the confines of a correctional facility," he said. "Knowing the folks that I know in the Department of Corrections, I know that that's in their hearts and minds, as well."
"I realize it certainly seems too slow a pace for people looking in, but this is a major shift in corrections," Menard said. "Ultimately, our biggest responsibility is to make sure that people in our care and custody are safe, so we need to make sure that we have everything in place to make sure that happens."
The commissioner said it's taken the DOC time to develop the right protocols for administering medication-assisted treatment. "It's difficult to manage a substance like that in your facility ... security-wise and safety-wise," she noted.
But Menard also acknowledged that, by now, they've worked out most of the kinks. And she emphasized that she's open to offering treatment for longer periods of time down the road.
Both Bick and Dalton believe medication-assisted treatment, and counseling, should be made available to any inmate struggling with an opiate addiction. They cite studies that have shown that 80 percent of inmates in state prisons in the U.S. have some type of substance use disorder. Their argument: Why not take advantage of having a captive audience that clearly needs addiction treatment?
"If you look at the science — and not everyone wants to look at the science ... it's hard to say there should be a time limit placed on somebody who happens to be incarcerated with this disorder," Brooklyn said.
"We know that the right amount of days is for as long as someone wants it and needs it," said Rep. Colburn. During this year's legislative session, she introduced legislation that would require ongoing treatment; it didn't make it out of committee, but she plans to try again in 2018.
By the DOC's own assessment, doing more would be relatively straightforward.
Its prisons would have to become federally accredited treatment sites to offer opiate medication to inmates who don't already have prescriptions. "My understanding is that the barriers to having a facility accredited as an outpatient treatment program are fairly low," Watts said. The main requirements: an alarm system, a safe to store the medication, a medication dispensing system and a designated space where the meds are administered.
Finding a room to do it in "is the biggest barrier, believe it or not," Menard said, noting that Vermont's seven prisons "weren't made spacious." Another factor: It takes staff time.
"We'll do what's requested of us," Watts said. "We just need the resources to do it, and we need the data to support that it's effective."
Blatt doesn't need numbers to know it makes sense. In September, he was out of prison on certain conditions, working, spending time with his 10-month-old daughter and taking his daily buprenorphine. But Blatt lost his spot in the sober house for a drug-dealing accusation that he denies. Now he's back in prison, being held because he doesn't have a place to live — a requirement for release. Last week, Blatt said corrections staff told him he'd soon be tapered off his bupe.
"I am so nervous and upset," he wrote, using the prison email system. "I just don't get how they can do this to me."
The original print version of this article was headlined "Cruel and Unusual?"
Related Stories
Got something to say?
Send a letter to the editor
and we'll publish your feedback in print!
Tags: Crime, buprenorphine, correctional facilities, Corrections, medication-assisted treatment, methadone, opiate addiction, Opioid Crisis, opioids, Suboxone
More By This Author
About The Author

Alicia Freese
Bio:
Alicia Freese was a Seven Days staff writer from 2014 through 2018.
Alicia Freese was a Seven Days staff writer from 2014 through 2018.
Speaking of...
-

'Safe Haven': Vermont Is Considering Controversial Overdose-Prevention Sites. 'Seven Days' Went to New York City to See One.
Mar 20, 2024 -

The Fight for Decker Towers: Drug Users and Homeless People Have Overrun a Low-Income High-Rise. Residents Are Gearing Up to Evict Them.
Feb 14, 2024 -

Backstory: The ‘Saddest Update’ on an Opioid-Addicted Source
Dec 27, 2023 -

Vermont Lawmakers May Have to Meet Growing Problems With a Shrinking Budget in 2024
Dec 20, 2023 -

A Program for Women Leaving Prison Struggles to Make the Grade at Middlebury
Dec 13, 2023 - More »
Comments (14)
Showing 1-10 of 14
Comments are closed.
From 2014-2020, Seven Days allowed readers to comment on all stories posted on our website. While we've appreciated the suggestions and insights, right now Seven Days is prioritizing our core mission — producing high-quality, responsible local journalism — over moderating online debates between readers.
To criticize, correct or praise our reporting, please send us a letter to the editor or send us a tip. We’ll check it out and report the results.
Online comments may return when we have better tech tools for managing them. Thanks for reading.
- 1. Governor Makes Last-Minute Appeal to Delay Vote on Ed Secretary Nominee Education
- 2. UVM, Middlebury College Students Set Up Encampments to Protest War in Gaza News
- 3. Dog Hiking Challenge Pushes Humans to Explore Vermont With Their Pups True 802
- 4. Scott Official Pushes Back on Former State Board of Ed Chair's Testimony Education
- 5. Burlington Budget Deficit Balloons to $13.1 Million News
- 6. A Former MMA Fighter Runs a Wildlife Rehabilitation Center in Cabot News
- 7. Home Is Where the Target Is: Suburban SoBu Builds a Downtown Neighborhood Real Estate
- 1. Totally Transfixed: A Rare Eclipse on a Bluebird Day Dazzled Crowds in Northern Vermont 2024 Solar Eclipse
- 2. Zoie Saunders, Gov. Scott’s Pick for Education Secretary, Faces Questions About Her Qualifications Education
- 3. Don't Trash Those Solar Eclipse Glasses! Groups Collect Them to Be Reused 2024 Solar Eclipse
- 4. State Will Build Secure Juvenile Treatment Center in Vergennes News
- 5. Vermont Awarded $62 Million in Federal Solar Incentives News
- 6. Queen of the City: Mulvaney-Stanak Sworn In as Burlington Mayor News
- 7. New Jersey Earthquake Is Felt in Vermont News