Published May 29, 2018 at 10:00 a.m.
Last fall, when Betsey's 16-year-old son "Thomas" went from being a goofy, personable and happy-go-lucky kid to one who was quiet, introverted and irritable, she initially assumed that he was just being a normal, moody teenager. Plus, she thought, Thomas' sister had just gone off to college, and the two siblings were very close.
But after a bicycle accident in October left him with a serious concussion, Thomas' mood swings went from bad to worse.
"He became much more depressed, and it kept going downhill faster and faster and spiraled out of control," Betsey recalled. (The Chittenden County mother asked that her full name, and her son's real name, not be used to protect their family's privacy.) "He was sad and upset all the time."
By early January, Betsey and her husband noticed that Thomas was acting "very aggressive." He never threatened or hurt anyone else, she emphasized, but he banged on tables and punched walls.
Then one night in late January, Betsey went down to the basement and found Thomas tying a belt to the ceiling. She recognized immediately that he was trying to hang himself.
"He was a different person. It's like a force came over him," she recalled. "Even in his eyes, the way he looked at me, the way he talked to me, it wasn't him. Something else had taken over."
Betsey, who'd wrestled with her own depression five years earlier, knew immediately that her son needed professional help. She contacted First Call for Chittenden County, a 24-hour crisis hotline operated by the Howard Center in Burlington. A clinician directed her to bring Thomas to the emergency department at the University of Vermont Medical Center for a psychiatric evaluation.
Once they arrived, Betsey and her husband knew they had avoided tragedy and assumed that Thomas would now get the mental health treatment he clearly needed. But their nightmare had only just begun. Because all of the psychiatric inpatient beds for children and teens in the state were full, Thomas waited for five days in the emergency department.
Meanwhile, his depression worsened, Betsey recalled. Thomas was put in a windowless hospital room. A pediatric psychiatrist stopped by every day to see him, upped his antidepressant meds and prescribed something to help him sleep at night, when "the darkness" — the family's word for his depression — was at its worst.
Mostly, though, Thomas sat in his room with someone outside his door to make sure that he didn't try to harm himself. One day, he listened as a female patient screamed obscenities for hours.
"He had to watch a man die right across [the hall]," Betsey added. "Kids shouldn't have to witness that ... That didn't help his recovery."
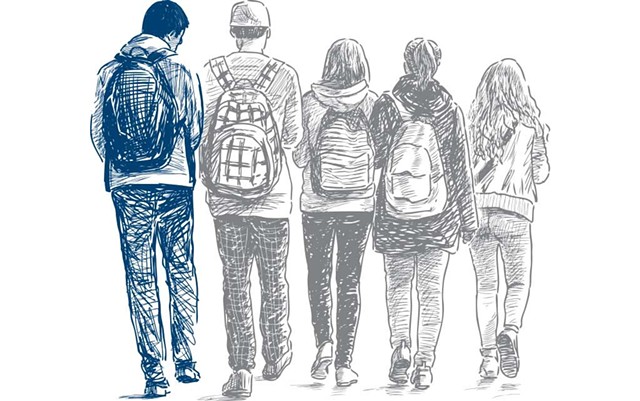
Thomas' story, though frightening, is not an anomaly. Children and teens who are suicidal or experiencing other forms of emotional or behavioral crises often wait hours, or days, in emergency departments for a psychiatric bed to become available, in part because most pediatric hospital units aren't equipped to provide psychiatric care. According to data from the Vermont Department of Mental Health, between October 2017 and March 2018, 157 kids in crisis waited in emergency rooms an average of 54 hours each for mental health placements. During that six-month period, one child waited 333 hours, or two weeks, for care.
One factor driving those long waits: a dearth of inpatient psychiatric beds for children and adults in crisis. The problem is more acute for kids because the state doesn't operate its own psychiatric hospital for children, like it does for adults. When suicidal youth are involuntarily committed — Thomas was not — often they're sent to the Brattleboro Retreat, a mental health and addiction treatment center in Brattleboro, or across the lake to Champlain Valley Physicians Hospital in Plattsburgh, N.Y.
Louis Josephson is president and CEO of the Retreat, which operates Vermont's only inpatient facility for children and teens 5 to 18 who've made a suicide attempt or are at serious risk of self-harm. Its 30 acute-care beds typically are for brief stays, averaging about a week, and are meant to stabilize a child so he or she can return home as quickly as possible.
The Retreat has another 24 beds for longer-term, less intense residential stays, which average about five months, for kids with chronic emotional or behavioral issues that cannot be safely managed at home or in foster care.
According to Josephson, the Retreat's longer-term residential care beds for kids are almost always full. Demand for the 30 short-term inpatient beds — the kind Thomas needed — tends to fluctuate seasonally, with peak demand from September through June. Only in the summer does the need subside.
Josephson, who's spent much of his career working with children and teens, said that when young people are in crisis and languishing in an emergency room, stress levels can skyrocket — for the patient, their family and the emergency department staff who are often "white-knuckling it until they can get [the child] over to us.
"Why is this acceptable?" Josephson asked. "You would never have someone with a heart attack sitting untreated in the hospital for a week. People would be up in arms. But somehow it's OK if you've made a serious suicide attempt."
The problem isn't unique to Vermont. Nationally, many states report long wait times for kids' psychiatric beds. The problem is further exacerbated by a nationwide shortage of pediatric mental health practitioners, including child psychiatrists, psychologists, and master's-level social workers and substance-abuse counselors.
With only about 30 child psychiatrists in Vermont, some kids wait weeks, if not months, for an appointment — though the Department of Mental Health has worked with practitioners to reduce those wait times, especially for youth in crisis.
Yet, by all measures, the workload is only increasing. Dr. Marshall "Buzz" Land Jr. is a pediatrician and professor of pediatrics at UVM Larner College of Medicine who's been in practice for 40 years. Over the last two decades, Land said, he's seen a significant decline in the number of kids coming in with serious physical ailments, such as tumors and infectious diseases, for which he credits the effectiveness of childhood vaccines and improved therapies.
During that same time period, however, Land said he's seen a 20 percent increase in the number of children who require inpatient mental health services.
"As those [physical] diseases drifted away, it became apparent to me that at least 30 to 40 percent of the kids who came through my door were coming in with a chief complaint of a behavioral mental health issue," he said. What's more, he added, the acuteness and complexity of those cases has also grown.
Land's personal observations have been confirmed by several national studies, as well as by conversations he's had with other pediatricians around the country as part of his work with the American Board of Pediatrics, the standard-setting body for pediatrics education and training.
Citing a 2014 report by the Robert Wood Johnson Foundation titled, "Are the Children Well? A Model and Recommendations for Promoting the Mental Wellness of the Nation's Young People," Land noted that about half of all Americans will experience a mental health problem at some point in their lives, most of which will originate in childhood.
The numbers are chilling: One in six high school students will consider taking his or her own life — and one in 13 will attempt it, according to data from the national Youth Risk Behavior Survey, conducted by the U.S. Centers for Disease Control and Prevention. Suicide is now the second leading cause of death in children 10 to 14, behind unintentional injuries, according to the CDC.
The forces driving the deterioration in children's mental health are numerous, complex and intertwined with other social problems, Josephson explained. Poverty and the opioid epidemic have left thousands of kids living in unstable, neglected and sometimes violent environments. Families often reside far from relatives and other support networks, who would otherwise lend a hand when problems arise.
"When a family is already close to being tapped out," Josephson added, "a young person with behavioral problems just tips everything over."
One Solution: Mental Health Care Starting at Birth
Some argue that one way to get kids who are in crisis out of the emergency rooms and into treatment is to invest in more inpatient psychiatric beds. Both Land and Josephson say that Vermont could benefit from having more short-term, inpatient beds for kids, especially in the northern half of the state.
But Melissa Bailey, commissioner of the Vermont Department of Mental Health, bristles at the suggestion that adding beds will solve the problem long-term.
"I've done this work for a really long time, and I've seen kids get put in residential [care], and that's where they stay for a very long time," she said.
Bailey, who started at DMH in 2001 in the Children, Youth and Family Services division and worked there for nine years before becoming commissioner in 2017, said that Vermont is actually doing better than most states when it comes to delivering mental health services to its kids and addressing its shortage of mental health care professionals. In 2009, she noted, the UVM Larner College of Medicine launched a child and adolescent psychiatry fellowship to provide specialized training to doctors. To date, of the 11 fellowship recipients to graduate from the program, eight have stayed in Vermont to work as child psychiatrists.
Bailey didn't refute that having kids in crisis stuck in emergency rooms, rather than in inpatient treatment, is a serious concern. Ultimately, though, she's focused "more upstream," she said. Her goal is "to prevent that need from existing in the first place."
To do so, she explained, means putting greater emphasis on prevention and early interventions at the community level, to stop small crises from becoming bigger ones.
One logical place to start is by working with the health care professionals who see kids most often and at the earliest age: pediatricians. Unfortunately, as Dr. Land pointed out, many of these doctors feel ill-prepared to treat, or even recognize, kids with mental health disorders when they come through the door.
"We know that 65 percent of pediatricians say [in national surveys] that they are not trained to take care of behavioral mental health problems and 44 percent don't even want to," Land said. Why? "They don't feel comfortable because they lack the training. And, they're not being reimbursed adequately for it."
Land, who's 73, no longer sees patients on a daily basis. Instead, he's made it his mission to ensure that the next generation of pediatricians, whether they're coming from UVM's Larner College of Medicine or other medical schools, get the mental heath training they need. His goal: to incorporate mental health instruction into every component of the three-year pediatrics residency. Currently, aspiring pediatricians get, at best, a one-month developmental-behavioral rotation as part of their residency, which some of them view as less important than the rest of their training.
"A huge percentage of residents take their vacation time during that month," he added. "It's just a terrible training system."
What would integrated training look like? Sometimes, Land said, it's just a matter of teaching residents to ask their patient, "How are you feeling?"
For example, when a doctor working in the emergency room sees a child with a broken arm, Land explained, he or she shouldn't just order an X-ray and apply a cast. The doctor should try to determine why that injury occurred and what its long-term consequences may be: Was this child bullied at school? Is there domestic violence at home? Is this a sports injury that may have been this student's scholarship ticket to college? And, now that she won't get to play in the big championship game, is she at risk of depression?
Land readily acknowledged that it's an uphill battle convincing medical school program directors to incorporate mental health training into every component of their pediatrics residency. Nevertheless, he said, the problem is too big to ignore.
"This is one-third of the kids coming through your door. And they're easy kids to overlook because they're complicated cases," Land argued. "If polio broke out in the United States right now, we're not going to tell the American public that we don't know how to treat polio. We're going to figure out how to teach [doctors] to treat them, fast."
Another Solution: Reconnect Mind and Body
When Vermont mental health commissioner Bailey talks about prevention, one model she cites is the Vermont Center on Children, Youth and Families at UVM, which treats kids and adolescents with emotional and behavioral disorders, along with the families of those referred. It's a program in high demand, with wait times up to a year.
Dr. Jim Hudziak, who runs the program, is a professor of psychiatry, medicine, pediatrics, and communication sciences and disorders at the UVM Larner College of Medicine. As he explained in an interview with Kids VT earlier this year, he and his team won't prescribe any psychiatric medications to young people before they — and their parents or caregivers — are engaged in therapy.
"First, we'd look at you [the parent] and your partner's emotional strengths and weaknesses," he explained. "If you have strengths, we build on them, and if you have weaknesses, we take care of you two first."
While the parents receive counseling, he continued, the child receives violin lessons, yoga and mindfulness classes, nutrition and sleep training, the assignment of a mentor and a physical activity tracker, such as a Fitbit, to reward daily exercise. Hudziak called it "health promotion by building healthy brains."
In the past, he noted, some critics dismissed this approach as "crunchy Vermont thinking." Not anymore.
"I wouldn't have all these violin lessons going on here unless there were sound brain science to back it up," he said. "If we can get kids to exercise seven days a week, we can reduce suicide attempts by 23 percent. There's no medicine that does that. And yet, in our country, we're so exercise-phobic when it comes to our children, it's hard to get parents to say, 'Get out there and exercise for an hour a day.'"
Thomas benefited from this kind of holistic approach. After waiting five days in the emergency room, no inpatient beds had opened up. So Betsey and her husband took their son home and watched him around the clock. They locked up anything in the house that was potentially dangerous and had Thomas sleep in their bedroom with them. Both parents are self-employed and were able to take time off from work to ensure his safety.
Four days after Thomas came home, Betsey got a call from Northeastern Family Institute, a private, nonprofit agency that runs a residential group home in South Burlington called Allenbrook. The eight-bed facility — which primarily serves kids 11 to 18 who are in the custody of the Department for Children and Families or those, like Thomas, who are on Medicaid — had a bed available.
Betsey jumped at opportunity, she said, because she knew that if they didn't, someone else would take that bed.
"It was a wonderful program," Betsey recalled. Thomas' day was very structured and included classes in yoga and meditation, which, his mother admitted, didn't always appeal to the teenager. Still, the group home allowed him to have visitors during his nine-day stay; one night, his parents even took him out for dinner.
Thomas returned home in mid-February, and after a short "honeymoon period," she said, he suffered another emotional setback, which resulted in another call to the crisis hotline.
As they worked through that incident, Betsey and her husband learned of a previously unknown trauma their son had endured: While Thomas was working at a local restaurant during his school winter break last year, an adult coworker had exposed himself and grabbed his genitals, then threatened Thomas if he told anyone. Suddenly, Betsey said, her son's suicide attempt began to make more sense.
In many respects, Betsey knows that she's more fortunate than many parents in the same situation. Medicaid covered her family's six-figure medical bills, most of which accrued during Thomas' five-day stay in the emergency department, as well as his nine days at Allenbrook. Moreover, because she and her husband are well-educated, they knew how to advocate for their son and get him treatment in ways that some parents cannot.
After missing a month of school, Thomas returned to classes and is doing well. He's still receiving therapy and taking antidepressants, but his pediatrician told Betsey he may only have to take the medication temporarily. "If this is what gets him through the day," she said, "so be it."
Betsey knows from her own experience with depression that this may be a long-term struggle for her son, albeit one that he, too, can overcome. She's just thankful that they got the opportunity to answer his cry for help.
"I was one of the lucky ones. He was one of the lucky ones," she said. "It could've ended a lot differently."
This article was originally published in Seven Days' monthly parenting magazine, Kids VT.
More By This Author
Speaking of...
-

Rep. Anne Donahue Is Determined to Find Out Where Patients of Vermont’s Old Psychiatric Hospital Are Buried
Mar 20, 2024 -

Noah's Arc: Noah Kahan Is Vermont's Biggest Cultural Export in Years. How the Hell Did That Happen?
Jan 31, 2024 -

Vermont Colleges School Students on Wellness as Mental Health Concerns Mount
Jan 17, 2024 -
Afterglow Music Festival to 'Shine the Light on Suicide Awareness'
Sep 18, 2023 -

A Young Man's Path Through the Mental Health Care System Led to Prison — and a Fatal Encounter
Sep 6, 2023 - More »
Comments
Comments are closed.
From 2014-2020, Seven Days allowed readers to comment on all stories posted on our website. While we've appreciated the suggestions and insights, right now Seven Days is prioritizing our core mission — producing high-quality, responsible local journalism — over moderating online debates between readers.
To criticize, correct or praise our reporting, please send us a letter to the editor or send us a tip. We’ll check it out and report the results.
Online comments may return when we have better tech tools for managing them. Thanks for reading.